Abstract
Introduction: The incidence of multiple myeloma (MM) increases with age. Novel agents provide better treatment results. However, adults >65 years of age are often underrepresented in clinical trials making it difficult to assess treatment outcomes in older patients. Appropriate strategies are necessary and treatment must be individualized in this heterogeneous population.
Methods: We retrospectively reviewed the charts of 534 patients diagnosed with MM between January 2010 and January 2020 who presented to our department. One hundred twenty-three of them were aged 65 years or older at diagnosis and were included in the study. Clinical and laboratory data were collected and potential prognostic factors of overall survival (OS) were evaluated by univariate and multivariate analyses.
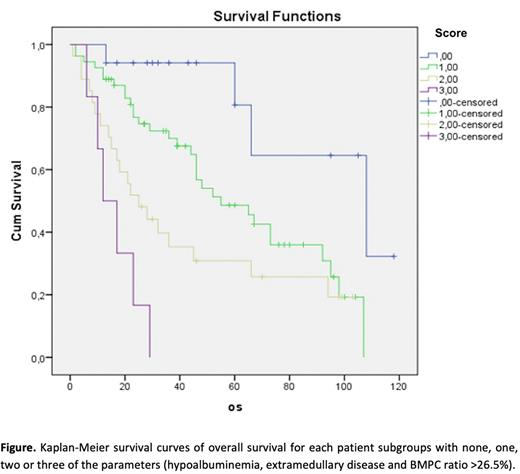
Results: Of 123 patients analyzed 54.5% (67) were male and 45.5% (56) were female. The median age was 71 years and 32.5% of patients were equal or older than 75 years. Median follow-up time was 28 months (1-117). Median OS and progression free survival (PFS) were 46 and 17 months, respectively. Of the patients 63.4% (78) died during the study period. The patients were divided into 3 groups according to age: 65-69 (47 patients, median OS 68 months), 70-74 (36 patients, median OS 45 months) and ≥75 (40 patients, median OS 36 months) years old (p: 0.022). International Staging System (ISS) stage could be defined in 117 patients (19 had ISS I, 40 ISS II and 58 had ISS III disease). Revised ISS (R-ISS) could also be defined in 117 patients (17 R-ISS I, 82 R-ISS II and 18 R-ISS III). Both ISS and R-ISS could not identify statistically significant differences regarding OS and PFS. Chromosomal abnormalities were detected by fluorescence in situ hybridization (FISH) and conventional cytogenetics in 56 and 39 patients respectively. Eleven of 56 patients and 4 of 39 patients had unfavorable genetic features and due to the small number these patients are not included in the survival analyses. Bortezomib based doublet and triplet induction regimens were given in 86% of patients. Univariate analysis revealed that age, hemoglobin, creatinine, calcium, albumin, extramedullary disease and bone marrow plasma cell (BMPC) percentage were strongly associated with OS. Receiver operating curve (ROC) analysis determined the optimal cut-off value of BMPC 26.5%. On multivariate analysis albumin, extramedullary disease and BMPC ratio retained prognostic value. Presence of none, one, two or all three of these factors could identify 4 patient subgroups showing median OS rates of 108, 55, 25 and 12 months, respectively (p: <0.001) (Figure).
Conclusions: MM primarily affects older adults. Hence, there is a need for simple and reliable staging systems for elderly MM patients. We propose a prognostic scoring method for outcome incorporating easy to use variables such as albumin, extramedullary disease and BMPC ratio. Hypoalbuminemia (≤ 3.5 g/dl), presence of extramedullary disease and BMPC ratio ≥ 26.5% predicted different OS ratios in the study population. A validation of the score in an independent series of patients is planned.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal